Years ago, scientists realized the potential for stem cells to be used to regenerate entire populations of damaged and dead cells afflicted with disease, an inevitable revolution in medical science. Stem cells, however, have been proven to be much more complex than originally thought. It has been a long journey for scientists all around the globe through collaboration and a lot of lab work, in order to master the complexity of the workings of stem cells. The next step would prove to be just as challenging, if not more so – that is, to apply the knowledge of the capabilities of these cells for use in medicine.
University of Rochester Medical Center scientists Steve Goldman, M.D., Ph.D., Maiken Nedergaard, Ph.D., and Martha Windrem, Ph.D., conclude that researchers are on the threshold of human application of stem cell therapy to myelin disorders, a class of neurological diseases. Examples of such diseases would be multiple sclerosis, white matter stroke, cerebral palsy, dementia, and pediatric leukodystrophies (a fatal childhood condition). There are many potential opportunities for clinical applications of stem cell research in areas such as central nervous systems (CNS) diseases, originating in the brain. These diseases are difficult to treat due to the complexity of the human brain, but it is postulated that the best outcome may come from the simplest cell types.
Oligodendrocytes are a common factor in myelin disorders. These cells come from alial progenitor cells, and the family has a “relative” which comes from the same cell, the astrocytes. These two cells are critical to the working functions of the CNS. They look to maintain neurons, and more specifically the axons as well. Oligodendrocytes help to build the fatty sheath (known as the myelin sheath) responsible for improving the efficiency in conductivity of signals between neurons, and astrocytes work hand in hand with these cells.
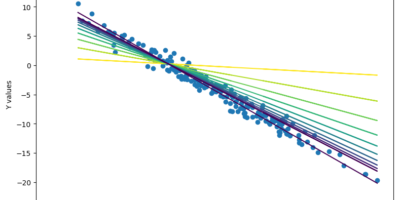
Cells such as the glial progenitor cells are the main target for stem cell therapies as they may be more readily manipulated and are easy to transport into the animal/human. It is shown that once injected into the animal, Oligodendrocytes work to “re-myelinate” damaged neurons. Dysfunctional glial cells lead to a broad spectrum of diseases and negative side effects, such as the degeneration of white matter due to age. Glial progenitor cells are easy to manipulate for use because one does not need to worry about targeting every single point-to-point connection between the neurons – the injected cells essentially direct themselves to these points. We can take advantage of this fact and introduce competent glial cells to the patient through direct transplantation in order to treat disease. This is all possible due to advanced MRI scanning technology, which provides scientists a clear image as to the results of their work.
Major advancements have been made, and large obstacles overcome in scientists’ abilities to control and manipulate such cells. Goldmans’ lab have been making pioneering efforts to pinpoint the chemical signals required to recreate glial progenitor cells from stem cells, then consequently instructing those cells to make either astrocytes or oligodendrocytes. Controversially, stem cells have traditionally come from embryos, but the stem cells used to recreate the progenitor cells in the lab have come from skin cells instead. Advancement in integration into neuronal networks has also been made, such as in Nedergaard’s lab. In his lab, Nedergaard and his team were able to integrate such cells into adult nervous systems, and were able to image the results afterwards.
These labs have furthered the possibility of using such therapies – glial progenitor cell transplants – on humans with dysfunctional glial processes instead of just animals. The labs have also provided sufficient models for such an advancement through advanced imaging technology. An example of a human disease that such a technique may help cure would be multiple sclerosis. The damaged fatty insulating sheaths of the nerve cells tend not to grow back once disintegrated. However, with the introduction of glial progenitor cells, the previously permanently damaged fatty sheathes will be able to be regenerated.


Leave a Reply